Kick-start your Professional Services
Stuck in a professional services rut? Or simply not sure how to start? This webinar recording is intended for both pharmacy owners and pharmacy managers.
We show you:
- How professional services can significantly increase the bottom line of your business;
- how to address the road blocks to implementing services within your pharmacy; and
- the tips and tools to improve the delivery of the services within your pharmacy.
*Please Note: This webinar makes reference to the Chronic Pain MedsCheck Trial, which has now ended.
PPA Claiming Checklist & Documentation Requirements for 6CPA programs
The Pharmacy Programs Administrator (PPA) has announced that, from the 1 February 2020, they have commenced active monitoring and compliance activities. PPA and the Department of Health will be ensuring pharmacies receiving funds for provision of 6CPA services are abiding by the Program Rules and are compliant with the PPA General Terms and Conditions.
Download our free PPA Claiming Checklist to help ensure your pharmacy is compliant*.
*This is a summary only, please refer to the PPA program guidelines for exact requirements.
How to create a MedsCheck friendly pharmacy
Follow these four simple steps to creating an efficient and effective MedsChecks workflow in your pharmacy.
1) Patient Flow
2) Teamwork
3) Resources available
4) Patient’s perceptions
Step 1) Patient Flow When implementing professional services within your pharmacy one of the first steps to take is creating the right environment.
The environment involves:
1. Physical environment for patients
2. Cultural environment between staff members (both pharmacists and pharmacy staff)
3. Location of professional service resources
4. Cultural experiences of patients (patients acceptance of receiving medication counselling in a new environment)
If the physical environment within the pharmacy does not facilitate a seamless experience for the patient, a pharmacist may find it difficult to guide patients into the pharmacies consulting room enabling a MedsCheck to be conducted.
Often only a few small changes are needed such as, changing the location of the patient waiting area/chairs, moving the prescription in or prescription out counter and or the location of the tills.
Here are some examples:
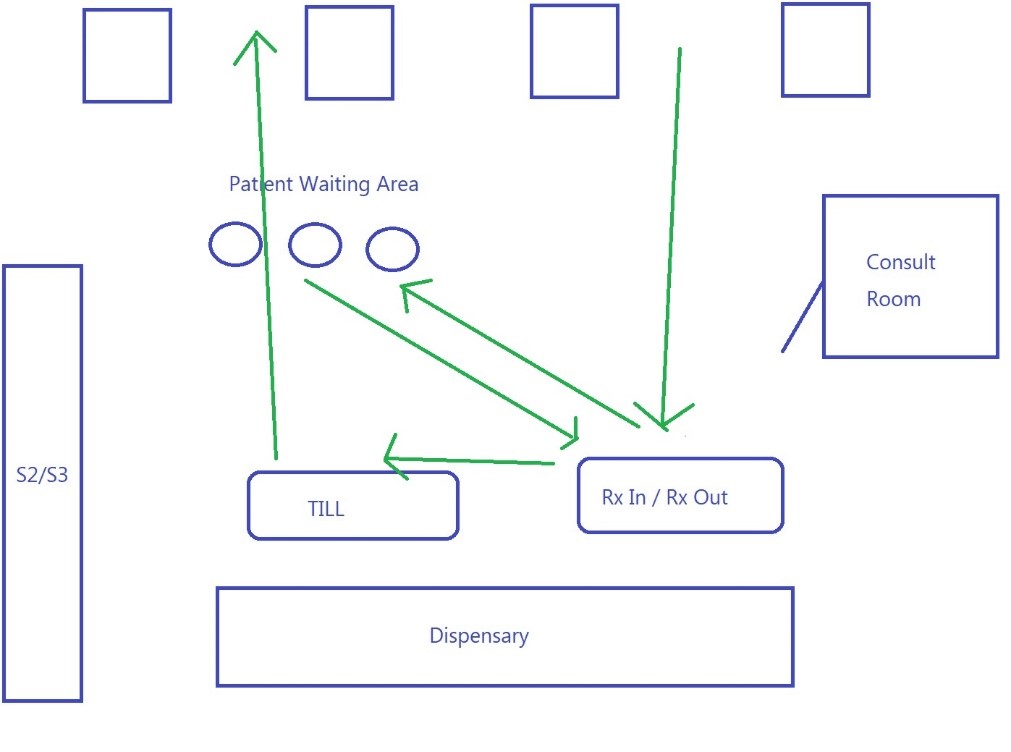
Current customer flow for prescriptions:
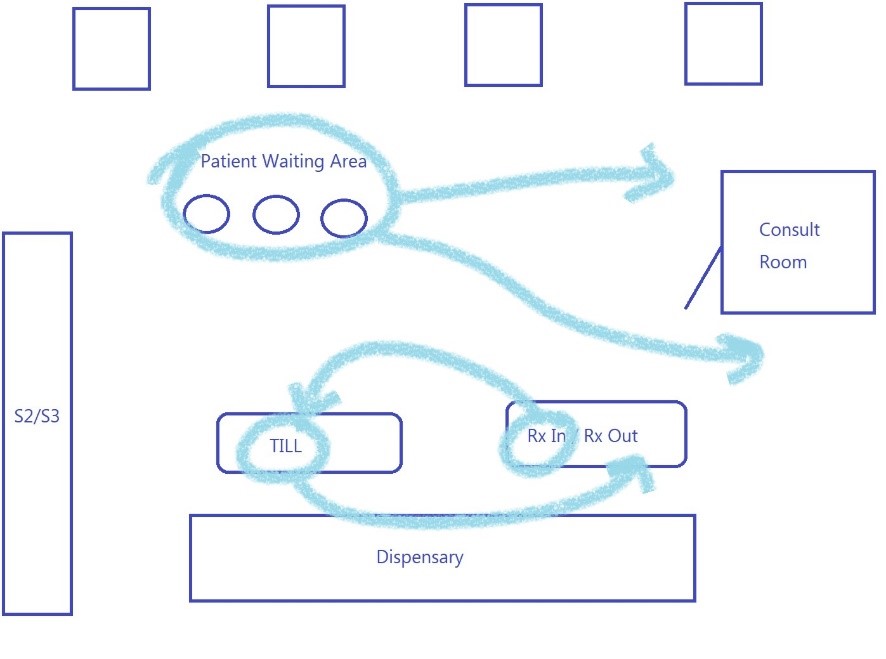
Recommended Changes:
Move the patient waiting area closer to the consulting room and closer to the prescription out counter Move the prescription in counter away from prescription out counter to prevent congestion and improve patient privacy
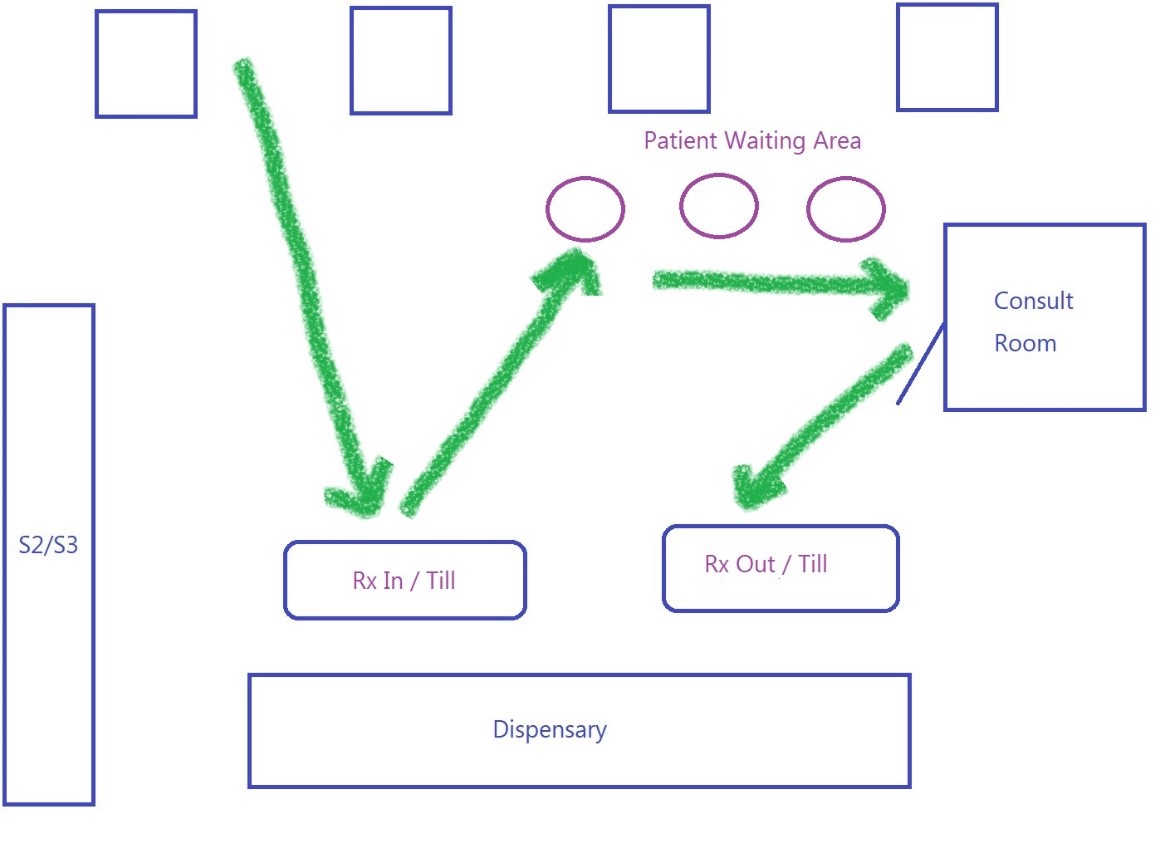
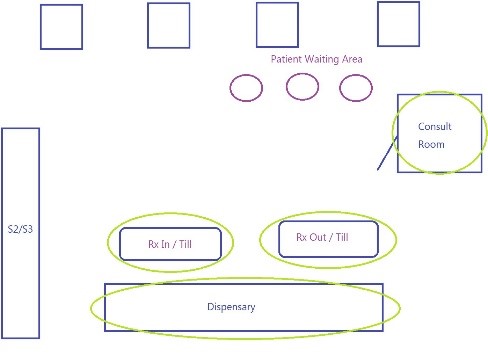
Recommended Layout:
Step 2) Teamwork Working together as a team to support the implementation of professional services
“Talent wins games, but teamwork and intelligence wins championships.” – Michael Jordan
Getting a team to work collaboratively together requires a lot of work, both from a manager/pharmacist in charge and team members/pharmacist assistants. Some of the more basic requirements include open communication, clear group goals and a clear vision.
Get to know each other
It is important that each team member knows each other and not just by their names or their job title. The team needs to know team members values, goals, strengths and the way they work. Once everyone knows this about their colleagues, it will be easier to define how to work best together.
Have clear goals and a clear vision
When the team members know each other, they can start working towards a shared goal. Supporting pharmacists to provide patients with 6CPA Professional Services. Make sure everyone in the team views the goal in the same way and how to achieve the goal.
Team members often have different visions regarding the same result. It is hard to work toward one common goal when individuals have totally different visions, make all team members are seeing the same picture.
Define clear roles
Team members need to have a trusting relationship with each other to ensure everyone feels supported during busy periods and know where to go for additional support if needed. Collaboration will also improve when the roles of individual team members are clearly defined and fully understood.
Brainstorm with your team different scenarios that may occur in the pharmacy when implementing professional services and discuss how the team could work together.
Before the pharmacist sits a patient down in the consult room to do a MedsCheck:
o Who does the pharmacist need to notify
o How does the role of each team member need to adjust to support the pharmacist in providing the MedsCheck
The pharmacist is in the consult room doing a MedsCheck and a patient brings in a prescription to be dispensed:
o Who can dispense the prescription
o How can/would the pharmacist like to be notified a script has been dispensed and is waiting to be checked
When individuals within a team have a clearly defined and understood role, team members will feel they can do a significant portion of their work independently without relying on the pharmacist to direct each customer interaction, stepping in only when needed. Pharmacy assistants/dispensary assistants and pharmacists can focus on what they do best. Individual work is as important as teamwork itself so you may need to provide your team members with additional skills and training.
Every pharmacy is unique and the individual skills required will vary. The important thing is to create a smooth flow between individuals allowing them to exchange their ideas and utilise each other’s abilities.
It is crucial to maintain clear communication and continue to motivate each other, as well as giving each other space to develop individual’s skills.
Step 3) Resources Available Ensuring the resources needed to conduct a MedsCheck are easily accessible
He who is best prepared can best serve his moment of inspiration.
― Samuel Taylor Coleridge
Once your team is working together to support the implementation of MedsChecks within the pharmacy the next step is ensuring the team have the relevant resources needed. These resources need to be pre-prepared and in place prior a patient entering the pharmacy as any patient may benefit/be eligible for a MedsCheck. Without good preparation the work flow is compromised and MedsChecks are less likely to be conducted.
There are four areas in the pharmacy which require resources to be in place: Prescription IN counter, Dispensary, Prescription OUT counter and the Consult room.
Prescription IN counter
When a staff member collects a prescription from a patient, this is a good opportunity to obtain specific information from the patient that is important in conducting a MedsCheck, this includes:
- If the medication is new for the patient (identify if the patient may be eligible for a MedsCheck)
- If the patient would like additional printed information on the medication (patient may be eligible for a MedsCheck if they are confused about their medication resulting in medication non-adherence)
- Patient’s phone number
- Patient’s date of birth (it may be more appropriate to collect this information when the pharmacist conducts the MedsCheck and asks the patient to sign the patient consent form)
The pharmacy may choose to have a computer available at the Prescription IN counter to facilitate the recording of this information directly into the dispense software, alternatively the answers may be recorded on a pre-printed template listing these questions.
Dispensary
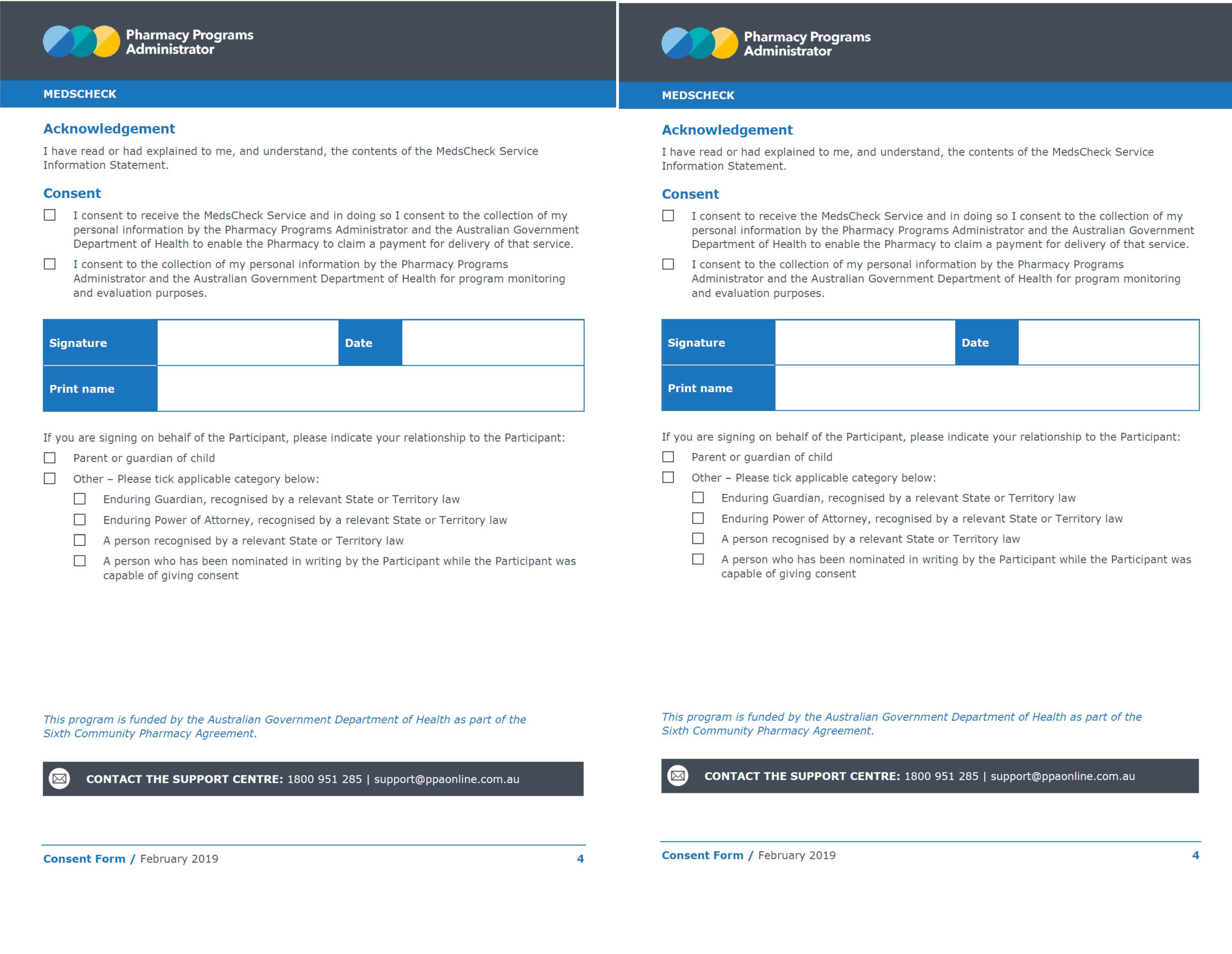
The dispensary plays an important role in identifying patients eligible for a MedsCheck through access to the patient’s dispense history and GuildCare pop-up prompts. When the dispenser (dispensary technician/pharmacist) has identified an eligible patient they can immediately place a MedsCheck patient consent signing form in the basket with the patient’s medication, along with the CMI if necessary. To ensure this happens, it is important to have the following resources pre-printed/available in the dispensary:
- Pre-printed A4/A5 MedsCheck patient consent forms
- Access to print CMIs or patient medication histories
- GuildCare open on dispensing computers (to ensure messages pop-up as reminders during the dispensing process)
One way of storing the MedsCheck patient consent forms in the dispensary is in a clear brochure holder.
Prescription OUT Counter
If the pharmacist checks prescriptions at the prescription out counter, the following resources are needed;
- Pre-printed MedsCheck patient consent forms
- Access to print CMIs or patient medication histories
- GuildCare open on dispensing computers (to ensure messages pop-up as reminders during the dispensing process
- Dispensary software open (to check patient details, dispense history)
- EMIMS or AMH open or bookmarked
If the pharmacist dispenses/checks prescriptions in the dispensary, the above resources may not be necessary to have at the prescription out counter, however, to improve the flow within the pharmacy, I would recommend ensuring the computer has easy access to everything listed above.
Consult Room
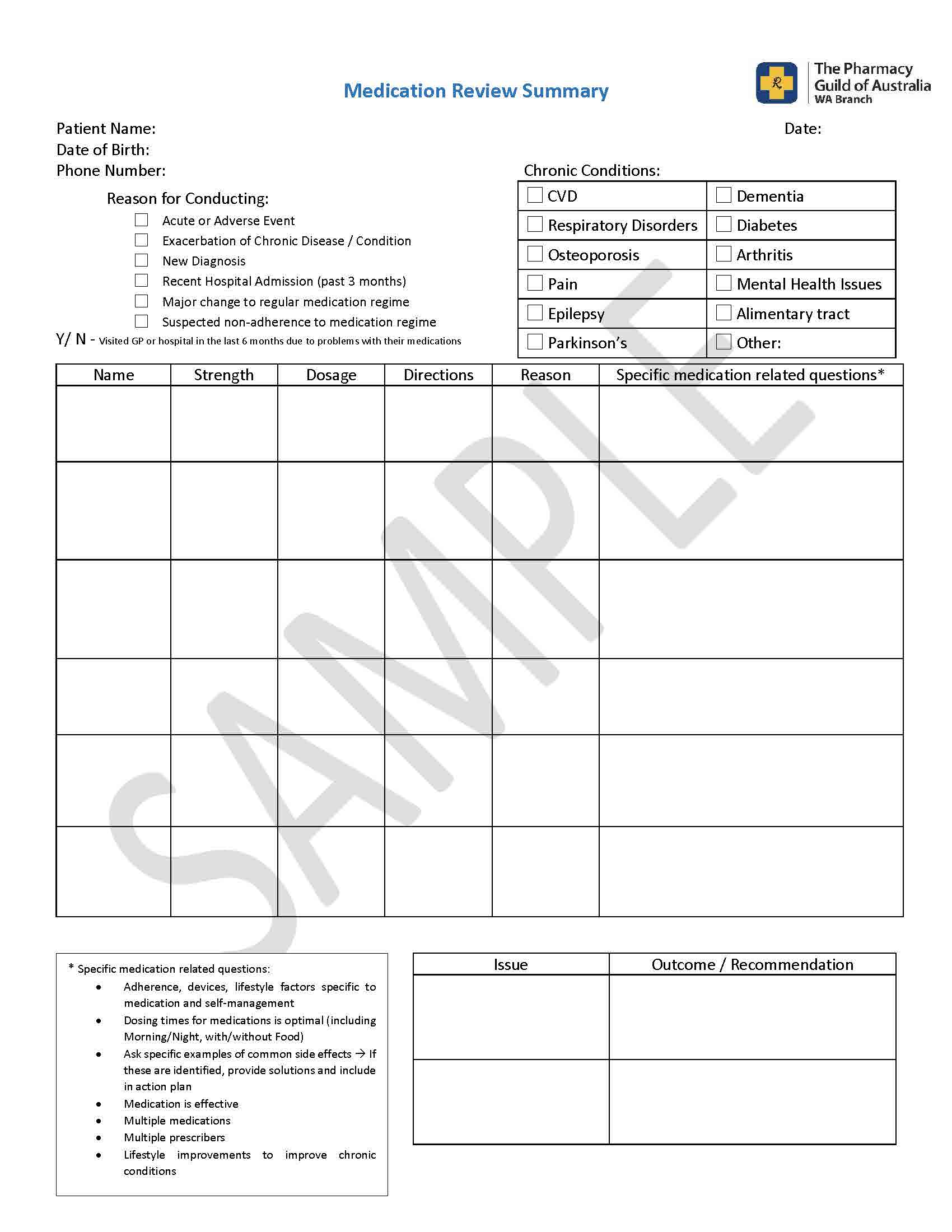
As not all pharmacies have access to a computer in their consult room, utilising a tool such as the “Medication Review Summary” template shown below may be useful in documenting the information discussed with a patient for recording in GuildCare at a later time. If this is something your pharmacy uses it is important to have this form pre-printed and located in the consult room as well as with the patient MedsCheck consent forms in the dispensary and prescription out counter.
Due to the individual operations of each pharmacy some of the above suggestions may not apply or may need to be adjusted to suit your pharmacy.
For electronic copies of the templates mentioned in this article, please contact Lucinda Crisp, Business Support Pharmacist lcrisp@wa.guild.org.au
Step 4) Patients' perceptions Creating a comfortable environment for patients to discuss their medications
“When we shift our perception, our experience changes” Lyndsay Wagner
As a pharmacist you are familiar with the terminology, processes and requirements involved in conducting a MedsCheck, however, your patients will not be. The implementation of the MedsCheck service within the pharmacy relies on your patients embracing change.
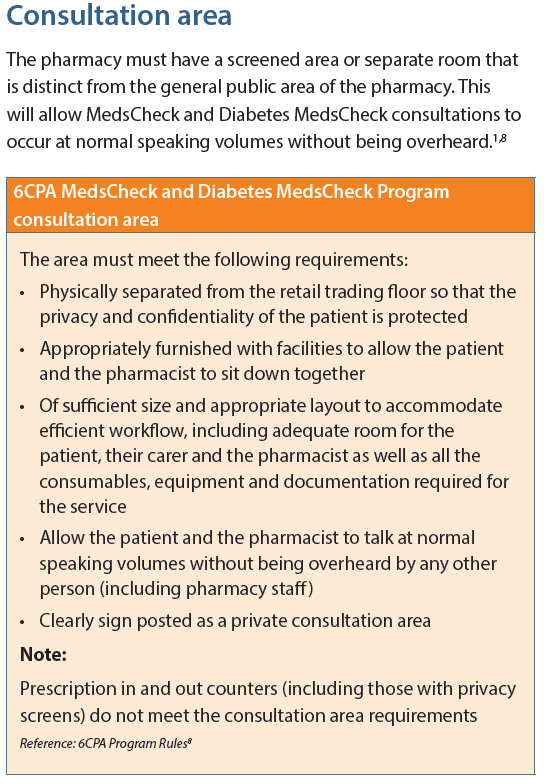
MedsChecks must be conducted seated, in a private area and physically separated from the retail trading floor (this excludes script in and out counters with privacy screens).
Most pharmacies have consulting rooms that are underutilised, resulting in patients holding a natural apprehension around being invited into the consult room. One way of allaying this apprehension is having all extended discussions with patients in the consult room.
When introducing changes to your pharmacy, patients will generally react in one of two ways. First of all, they might be receptive to the changes; this often occurs when the changes don’t require a large shift in attitude or behaviour and allows them to remain in their comfort zone.
On the other hand, patients may be resistant to change. This usually occurs when they have to adjust how they interact with your pharmacy. In this case, your patients will more likely develop negative perceptions towards the new changes.
Here are some measures we can employ to engage patients in the new process to help them feel at ease:
- Analyse the concerns from the patients’ point of view: The acceptance of the new change happens in the mind of the other person. Regulatory changes may seem easy to enforce, most patients aren’t that interested in the reasons why something needs to happen a certain way – they just want to have their needs met. Involve ALL your patients, use your consult room for all extended discussions with patients, not just with patients that may be eligible for a MedsCheck.
- Engage your patients in your pharmacy’s ecosystem: Often, one change within the system will impact other areas of the pharmacy. Think of your pharmacy as a complete ecosystem that is living and breathing. After completing a MedsCheck with a patient, ask them about their experience within the pharmacy's ecosystem.
- Build real intelligence: Make sure you are using the right metrics to measure the success of your new professional service offering. We might think of number of scripts dispensed as a success metric, however, this alone will not necessarily inform us if the new changes implemented are successful. If you completed a MedsCheck with a patient but the patient did not return for repeat prescriptions, is that a sign of success? Tracking ongoing patient engagement with your pharmacy will give you a clearer picture of how successful your new professional service was. One tool that you could use to track patient engagement is analysing your 6 month MedsCheck follow-up consultations, number/percentage completed (patient loyalty) and outcomes achieved (patient satisfaction).
- Manage expectations: Be clear with your patients about what they can expect through each step of their pharmacy journey. Don’t be afraid to make it simple and spell it out for them. For example: “Mrs Jones, I have your prescriptions ready, come with me and have a seat so we can discuss your medications/new medications/changes to your medications”.
- Develop a strong patient relationship: Remember, purchasing strategies have changed. Your patients have access to more choices than ever creating a significant challenge for pharmacies. Develop and maintain a strong relationship with them. Make your patient feel like you are on their healthcare team, and you are not simply dispensing a prescription and supplying a product. Tell them what they can rely on you for and what support/advice you will provide them with. Help them create ownership of their health by engaging them in new professional services in the pharmacy.